9-8-8 Fact Sheet
We are excited to introduce the 988 Suicide & Crisis Lifeline Fact Sheet! The 988 Lifeline provides compassionate, accessible care and support for people experiencing mental health-related distress.
The fact sheet is a valuable resource for community-based organizations and schools:
- Outlining the importance of shifting from a discipline response to a care-and-compassion response for students struggling with stress, depression or suicidal behaviors;
- Providing information on how 988 can be utilized by anyone experiencing mental health challenges, as well as by third parties concerned about a friend, student or loved one;
- Offering practical guidance on how schools can implement 988 as part of their suicide prevention and mental health policies and protocols.
Use this fact sheet to raise awareness about the 988 Lifeline! By sharing this resource widely, we can help ensure that individuals in need have access to the support and care they deserve.
Thank you to our partners in this effort: California Black Women’s Health Project, Didi Hirsch, and The California Alliance of Child and Family Services.

How Medi-Cal Continuous Coverage Protects California Kids
Making Medi-Cal Work for Families
Imagine being a parent to a 20-month-old and learning through a developmental screening that your toddler might have autism spectrum disorder. The pediatrician recommends a full diagnostic evaluation and early intervention services. But soon after that screening, you find out your child was dropped from health insurance coverage. While you work to re-enroll as quickly as possible, the process takes six months — during which time, your child cannot get any of the necessary follow-up care. And your distress is exacerbated!
As we witness California children losing coverage as Medi-Cal annual redeterminations start up again, TCP wanted to raise parent voices to speak to what are the very real impacts of gaps in health coverage on children and their families. We commissioned Lake Research Partners to conduct 10 focus groups with over 80 parents/guardians of children of color to share their experience with what it means to be without insurance coverage – even for a short period.
Listening to families themselves advances health equity by identifying how the process can work for them, not just for the system.
Learn more in our summary slide deck.
Advocacy for Implementation of Multi-Year Continuous Coverage in Medi-Cal
The Children’s Partnership and our partners for health equity have submitted multiples letters to California Governor Gavin Newsom to #KeepKidsCovered representing a diverse coalition of champions for young children through the Whole Child Equity Partnership and a coalition of child health advocates.
The letters are supported by state and local organizations requesting to fund and green-light implementation for continuous Medi-Cal coverage protection for young children in the Governor’s January 2024 budget.
TCP Brief on How Medi-Cal Continuous Coverage Protects California Children
A TCP brief, “Learning From the Pandemic: How Medi-Cal Continuous Coverage Protects California Kids,” calls attention to the positive impact that the continuous coverage provision has had in allowing millions of Californians to stay enrolled in Medi-Cal coverage during the COVID-19 pandemic and what is at stake for children and families when the protection ends in late March 2023.
The brief makes clear that the federal continuous coverage protection has:
-
significantly reduced coverage gaps for California children
-
protected access to care for children of color on Medi-Cal
-
served as a critical tool in improving Medi-Cal’s low preventive care rates
This brief also highlights recommendations to help the state minimize disruptions to children’s coverage, and urges DHCS to move forward with implementation of multiyear continuous Medi-Cal coverage for children ages 0-5.
One million CA kids are projected to lose their health coverage in the next year – mostly kids of color.
Here’s Why:
The federal continuous Medi-Cal coverage protection is ending March 31, 2023.
The Good News:
California has a new coverage policy that could protect children from losing coverage.
Why We Need to Take Action:
This policy is not slated to begin until 2025. This delay in implementation places thousands of children at risk of losing coverage unnecessarily.
How to Take Action:
Share this brief and ask the Governor to fund continuous coverage in the FY24-25 Budget.

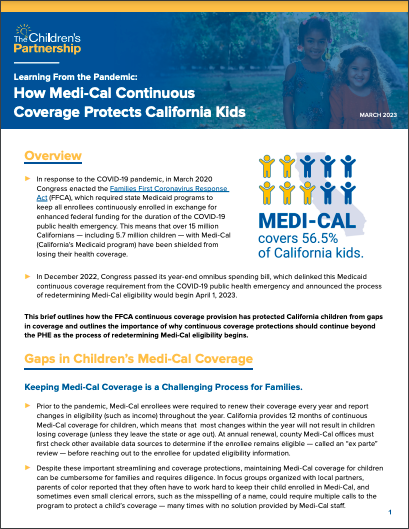
Feedback Loop
FEEDBACK LOOP
MEDI-CAL UNWINDING & RENEWALS RESTART
Monthly virtual opportunities to share your experiences with Medi-Cal renewals. Attendees can ask questions, get updates and share feedback.
Register here: https://bit.ly/RenewalFeedbackLoop
Do you work with California communities on Medi-Cal? Do you assist individuals and families with Medi-Cal enrollment and renewals? We are here for you and want to hear from you!
As Medi-Cal renewals resume, The Children’s Partnership (TCP) & the National Health Law Program (NHeLP) are hosting a feedback loop to identify and help address issues and concerns with the renewal process.
If you are a community-based organization, health care navigator, enrollment assister, community health worker/promotora, provider, or other advocate on the ground, please join us. Our virtual meetings will take place every month following December, starting at 12 p.m. PST:
- December 13, 2023
- January 24, 2024
- February 28, 2024
- March 27, 2024
- April 24, 2024
- May 22, 2024
Interpretation services will be provided upon request.
Please register here: https://bit.ly/RenewalFeedbackLoop
Questions?
Contact:
Kristen Golden Testa – ktesta@childrenspartnership.org
Skyler Rosellini – rosellini@healthlaw.org

NEW REPORT:
Telehealth and Children of Color with Special Healthcare Needs: Lessons from the Pandemic
Children of color and children in immigrant families make up over a majority of children with special health care needs (CSHCNs): 71% of the state’s CHSCNs also identify as Latinx, Black, Indigenous, Asian American, Pacific Islander, or Mixed Race, making up nearly 1 million children. Yet despite the size of their population, there is a lack of statewide research or policy focus on the needs of this population of children. TCP’s report, Telehealth and Children of Color with Special Health Care Needs: Lessons from the Pandemic, utilizes a community-centered approach to create a policy agenda that centers the lived experiences of families and children of color with special healthcare needs in California.
The learnings from the report provide unique insights into the experiences and challenges they and their families faced during pandemic shutdowns, including in the use of telehealth to access care. The report also sets forth actionable policy recommendations rooted in the experiences and recommendations of families of color with children who have special health care needs.

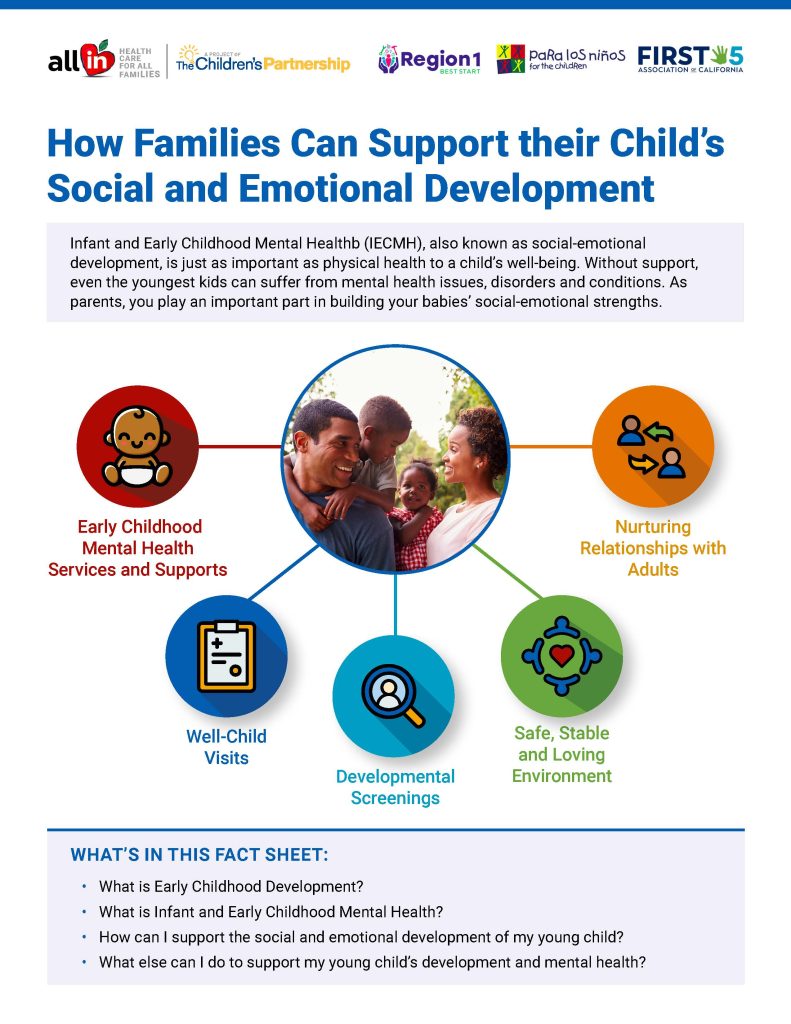
How Families Can Support their Child’s Social and Emotional Development
Infant and Early Childhood Mental Healthb (IECMH), also known as social-emotional development, is just as important as physical health to a child’s well-being. Without support, even the youngest kids can suffer from mental health issues, disorders and conditions. Parents play an important part in building your babies’ social-emotional strengths.
In partnership with First 5 Association of California, Para Los Niños and Best Start Region 1, we are releasing a new community resource: “How Families Can Support Their Child’s Social and Emotional Development.” This community resource is intended to help parents, caregivers and family members of infants and toddlers support their child’s early mental health and social-emotional development.

In partnership with the Latino Coalition for a Healthy California and Nourish California, we released a policy brief analyzing the drivers, consequences and impacts of food insecurity for Latinx children and families in California. The brief has an emphasis on the impacts of food insecurity on Latinx children and discusses the unique barriers to food access for undocumented Latinxs in California. Furthermore, it offers bold and feasible solutions that legislators and elected leaders can take now to address this issue for California’s largest ethnic population.
Californian Latinx individuals and families come from a wide variety of backgrounds, making us extremely diverse. Yet food insecurity is a pervasive issue among Latinx communities in California. In order to lead healthy and thriving lives, sufficient nourishment is an absolute necessity. Securing Food, Securing Our Health: The Impact of Food Insecurity on Latinx Children & Families analyzes the complex political and economic landscape that Latinxs in California face to access state and national nutritional assistance programs.

In the spring and summer of 2020, youth in the United States experienced a cascade of community trauma and stressors. The global COVID-19 pandemic swept through communities of color at alarming and disproportionate rates compared to white communities. The ensuing school closures, social isolation and dramatically reduced access to services and care, combined with the overall threat of the virus and the collective and individual grief over loved ones who died from COVID-19, have produced alarming mental health trends for young people. The public health crisis also coincides with horrific incidents of police brutality that have renewed momentum toward racial justice and healing in response to calls to action heard across the country. In light of the past year, with a devastating global pandemic and renewed momentum toward anti-racist policy solutions, the need for adequate, culturally responsive and gender affirming mental health needs is as apparent and urgent as ever.
In response to the historic and quickly escalating crisis of mental health for youth from marginalized communities, The Children’s Partnership (TCP) and the National Black Women’s Justice Institute (NBWJI) formed The Hope, Healing and Health Collective (H3 Collective), a youth-led policy council, with support and thought partnership from adult allies within policy, research and direct service and government, that developed a policy agenda to build the capacity of youth-serving systems to provide effective and compassionate care to young people and their communities.
The report, Youth-Centered Strategies for Hope, Healing and Health, sets forth actionable solutions that policymakers at the federal, state and local levels can implement to build a culturally-responsive and gender-affirming mental health care system for all youth, especially youth of color.

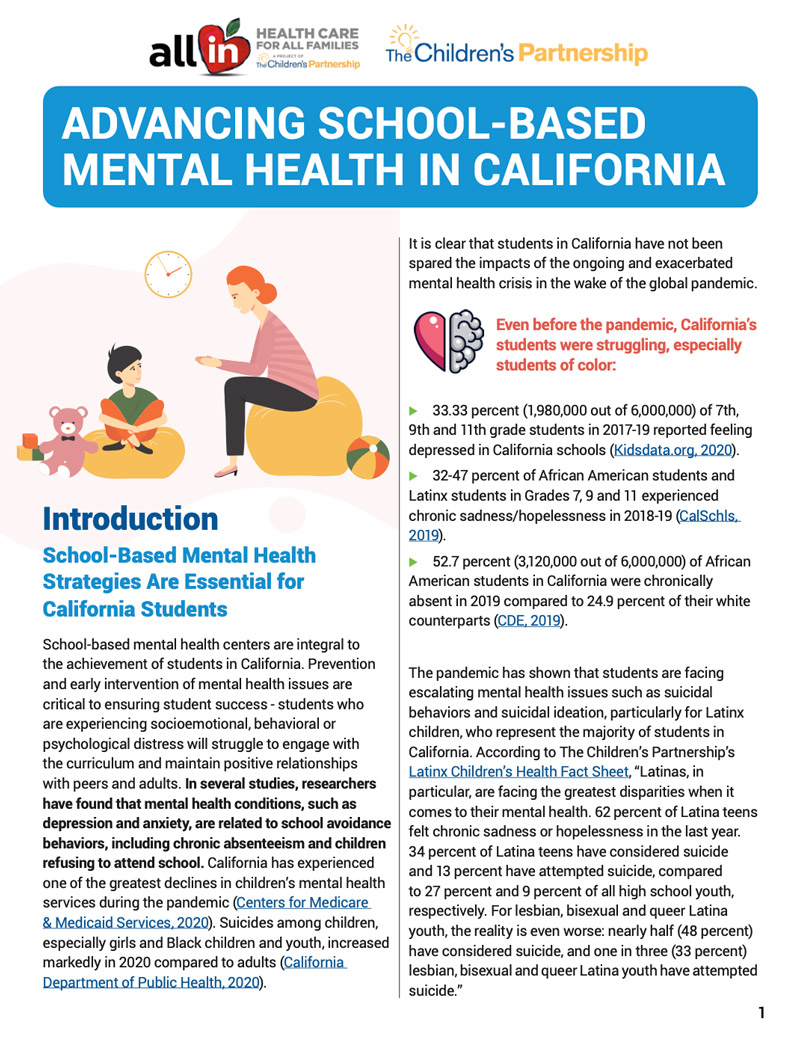
Advancing School-Based Mental Health in California
Prevention and early intervention of mental health issues is critical to ensuring student success – students who are experiencing socioemotional, behavioral or psychological distress will struggle to engage with the curriculum and maintain positive relationships with peers and adults. We know that when children are given the proper resources to thrive, they are more likely to succeed in school and in life.
In this brief, Advancing School-Based Mental Health in California, The Children’s Partnership (TCP) provides an overview of key components of school-based mental health models and includes data that demonstrates whole-child approaches to student success are integral to the achievement of students in California, especially students from marginalized communities.

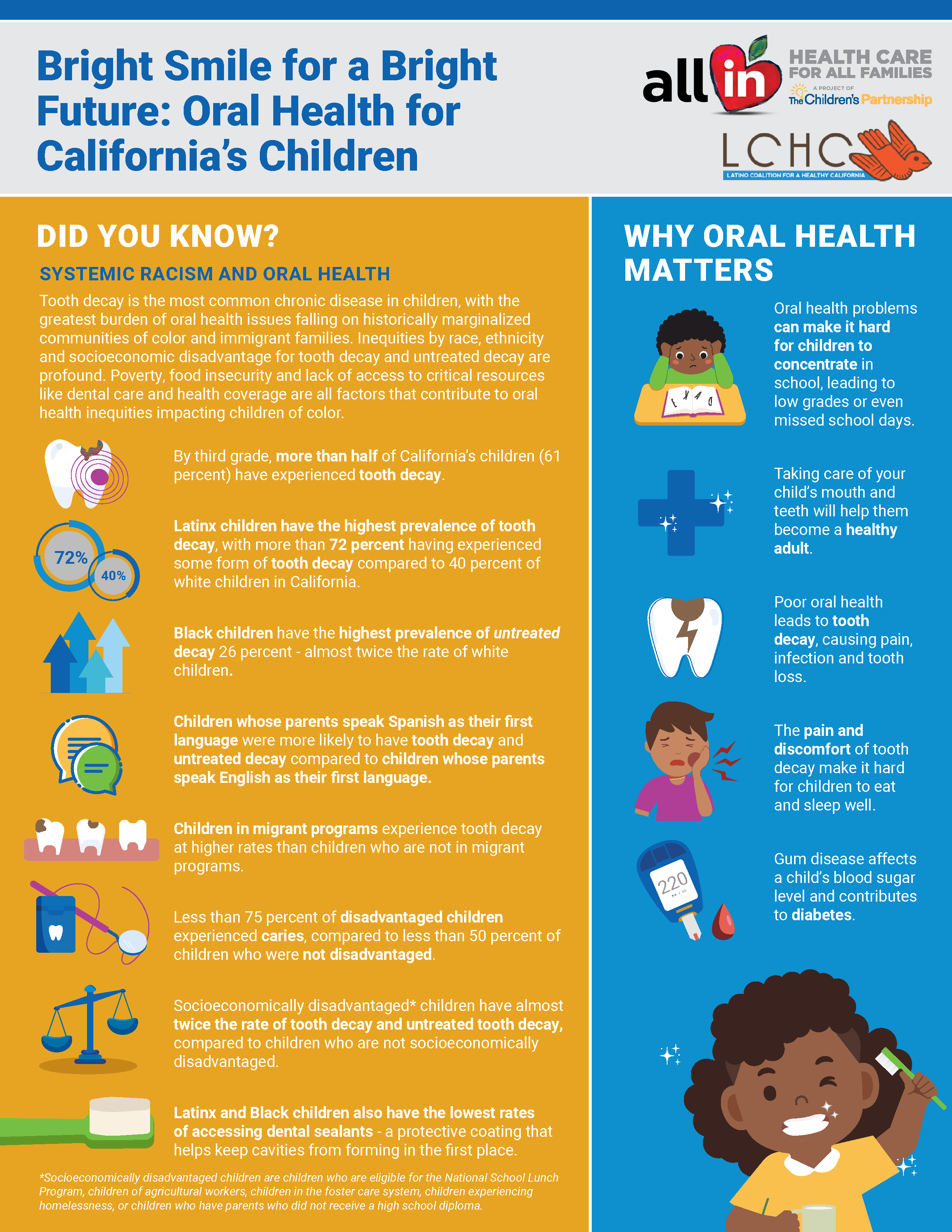
Tooth decay is the most common chronic disease in children, with the greatest burden of oral health issues falling on historically marginalized communities of color and immigrant families.
We partnered with the Latino Coalition for a Healthy California to create a two-page fact sheet that includes information to parents and families on why protecting the oral health of their children is important for their well-being and their future. We also share critical resources around accessing dental coverage through Medi-Cal and Covered California. Our fact sheet gives parents quick and easy tools to prevent tooth decay in their kids. Click below to access the fact sheet in either English or Spanish.
Help us uplift the content of this fact sheet to reach more parents and families by using our social media toolkit! Click here to access the toolkit.

Healthy Mind, Healthy Future
PROMOTING THE MENTAL HEALTH AND WELLBEING OF CHILDREN IN IMMIGRANT FAMILIES
Last year, The Children’s Partnership and the California Immigrant Policy Center joined efforts to launch Healthy Mind, Healthy Future, a research and policy project that aims to better understand the impact of heightened immigration enforcement activities and anti-immigrant rhetoric on the mental health and wellbeing of children in immigrant families in California, and identify what more California can do to support children in immigrant families.
Our new report, Healthy Mind, Healthy Future: Promoting the Mental Health and Wellbeing of Children in Immigrant Families, documents our research project, including results from focus groups and surveys among immigrant families, surveys among health care providers, and key informant interviews among a variety of stakeholders throughout California. The report also shines a spotlight on promising programs and practices in California that demonstrate how many schools, clinics, and community-based organizations in the state are taking matters into their own hands to help mitigate the increased fear and anxiety among immigrant families.
THE EFFECT OF HOSTILE IMMIGRATION POLICIES ON CHILDREN’S MENTAL HEALTH
Children of immigrants are the fastest-growing child population in the United States. They will be an increasingly important part of our workforce and will help subsidize Medicare and contribute to state and local economies. As California remains a change agent for our nation and immigrant communities, The Children’s Partnership and the California Immigrant Policy Center are combining efforts to examine the impact of immigration policies and actions on the mental health of children in immigrant families in California and identify what more can be done at the local, state, and national level to support the healthy development of these children. The release of the brief The Effect of Hostile Immigration Policies on Children’s Mental Health is the first in a series of initiatives to better understand what more we can do as a community to support the health and wellbeing of children in immigrant families. In the coming weeks, we will assess the impact of harmful federal policy changes on children in immigrant families in California. With commitment and leadership focused on sensible policy solutions, we can ensure that children in immigrant families remain healthy, feel secure, and continue to thrive.
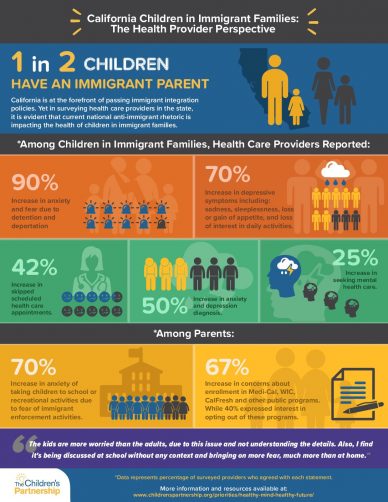
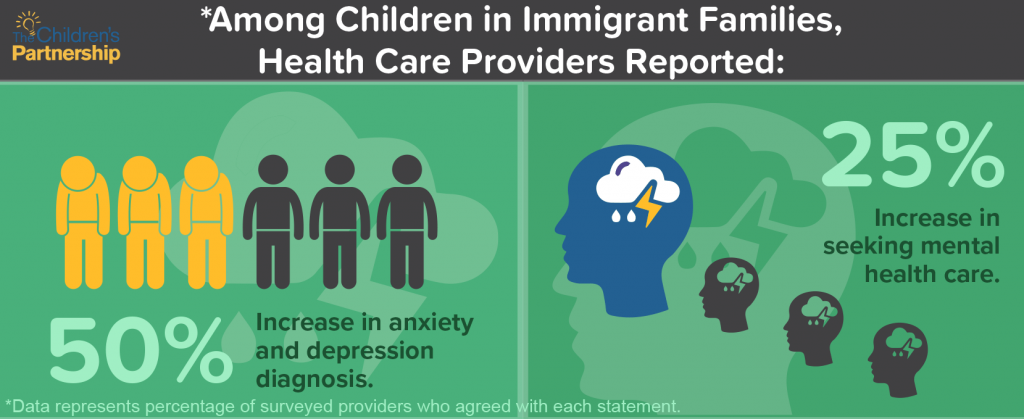
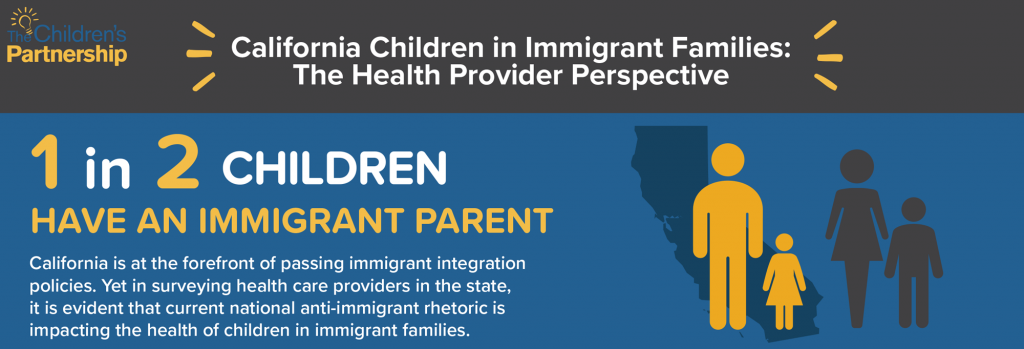
CALIFORNIA CHILDREN IN IMMIGRANT FAMILIES: THE HEALTH PROVIDER PERSPECTIVE
1 in 2 Children HAVE AN IMMIGRANT PARENT. California is at the forefront of passing immigrant integration policies. Yet in surveying health care providers in the state, it is evident that current national anti-immigrant rhetoric is impacting the health of children in immigrant families.
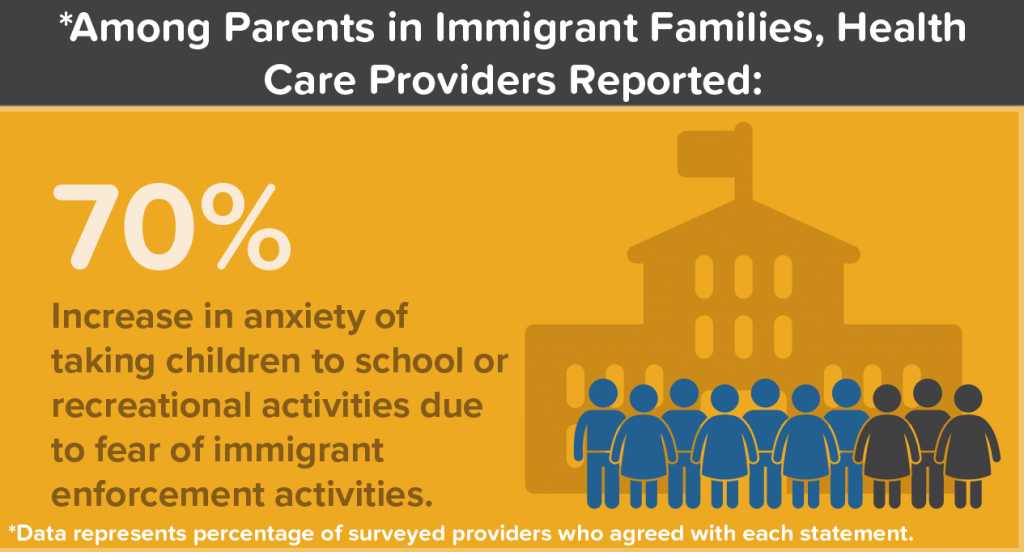
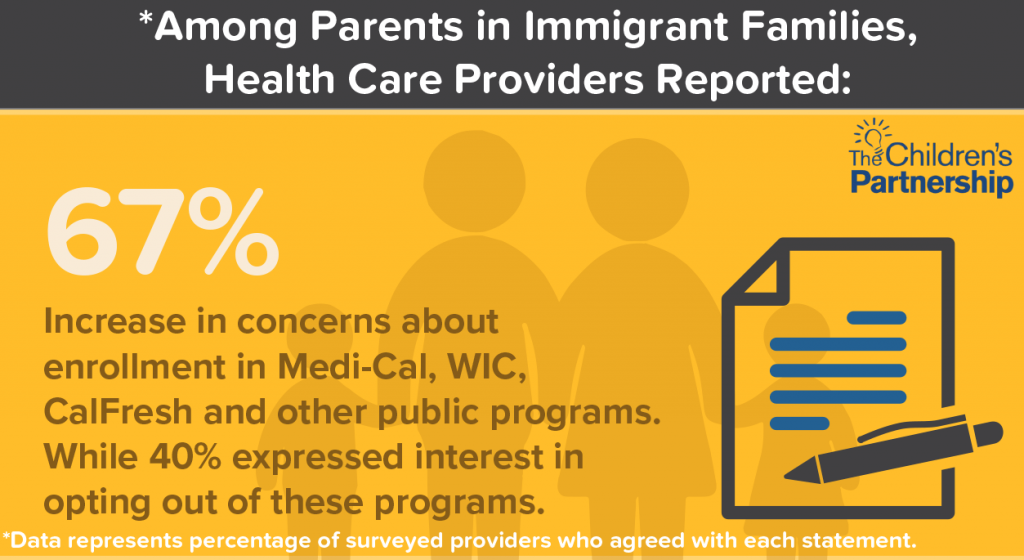
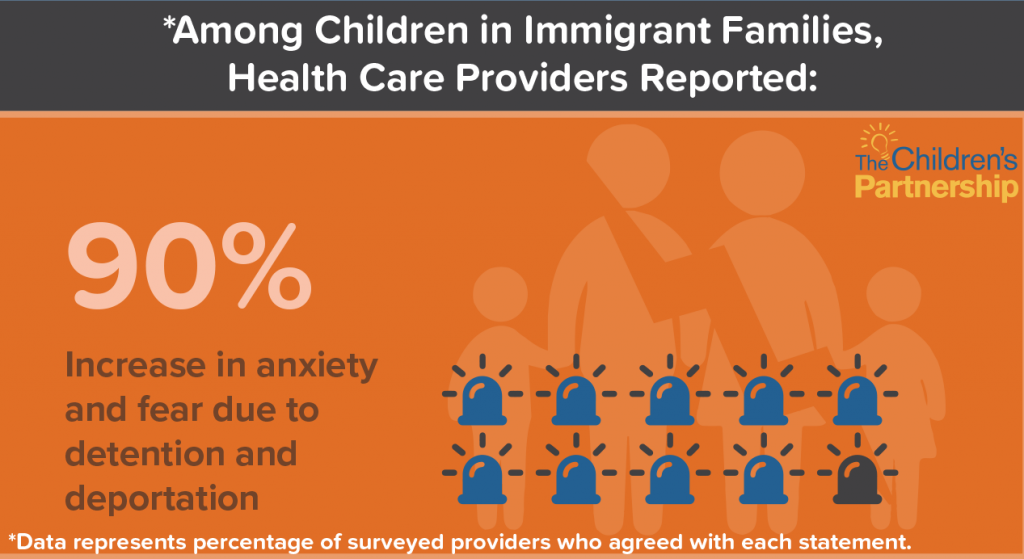
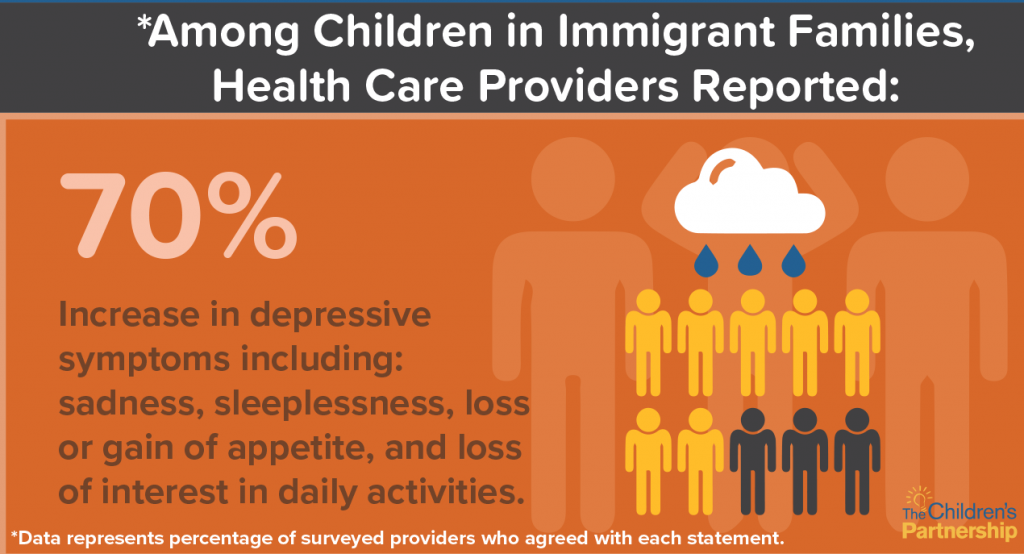
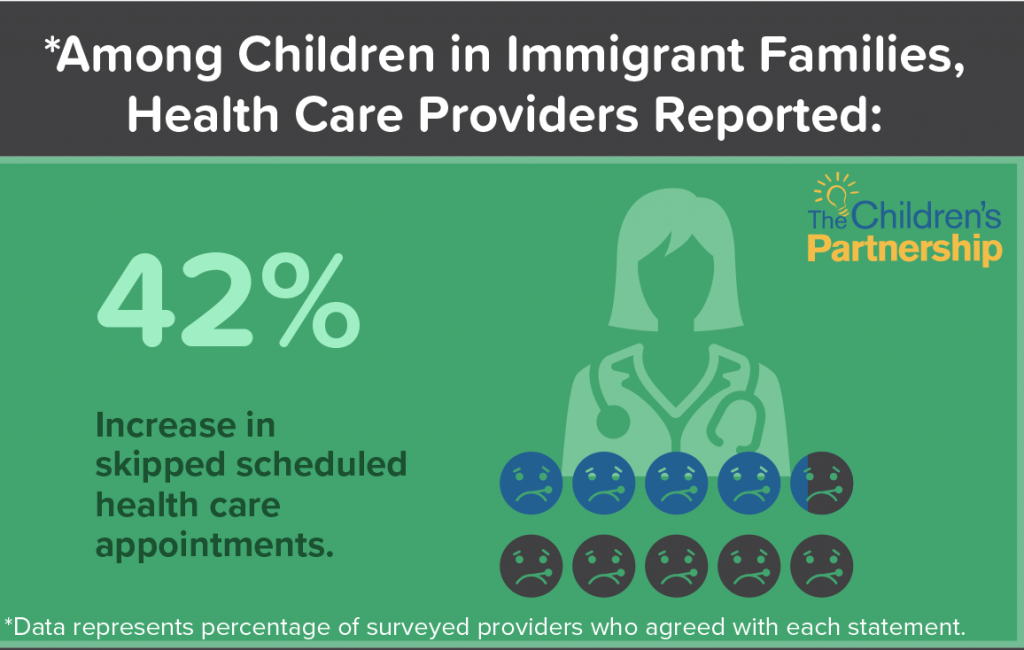
The Children’s Partnership commissioned a 27 question survey on immigrant children’s and families’ access to care and overall health. It was distributed to health care providers across California; 151 individuals who provide and coordinate health care services completed the survey. Survey respondents represented counties across the state with most being from Southern (n= 70, 50.4%) and Northern California (n=58, 38.4%). The survey asked respondents about a variety of topics related to changes in health care access as well as immigrant family health and wellbeing since the November 2016 General Election, and it also asked them to identify resources needed to effectively provide care to immigrant families. The percentages reflected in the one pager represent surveyed providers agreement with each statement*.
Data reflected in the one pager was rounded to nearest percentile. More details can be found here:
- Nearly 90% of providers stated that children in immigrant families experienced increased anxiety and fear due to detention and deportation (n=121, 87%)
- Over 70% reported an increase in children experiencing symptoms of depression (such as feelings of sadness, sleeping problems, loss or gain of appetite, loss of interest in activities they used to enjoy) (n=97, 72.4%)
- 42% reported children in immigrant families were increasingly skipping scheduled health care appointments (n=64; 42.4%),
- Nearly 50% of respondents stated that immigrant children are increasingly being diagnosed with mental health conditions such as anxiety and depression (n=76, 49.2%),
- Almost a quarter said that parents are increasingly seeking mental health care for their children (n=45, or 23.4%).
- Almost 70% of providers reported that immigrant families were increasingly expressing fear in bringing their children to school, the park, or recreational activities due to fear of immigrant enforcement activities (n=104, 69.4%).
- Two-thirds of respondents observed an increase in families concerns about enrolling in Medi-Cal, WIC, CalFresh or other public programs (n=101, 66.9%)
- While nearly 40% stated that immigrant families have increasingly expressed interest in disenrolling in Medi-Cal, WIC, CalFresh or other public programs (n=56, 37.6%).
This document is brought to you by The Children’s Partnership, The California Program on Access to Care (CPAC), California Primary Care Association, Dr. Cecilia Ayon, and the 151 providers who participated in the survey.


References
- Charmaz, K. (2006). Constructing grounded theory: A practical guide through qualitative analysis. Thousand Oaks, CA: Sage.
- Costello, M. (2016). After election day: The Trump effect// The impact of the 2016 presidential election on our nation’s schools. Southern Poverty Law Center, Retrieved from https://www.splcenter.org/sites/default/files/the_trump_effect.pdf
- Potochnick, S. R., & Perreira, K. M. (2010). Depression and anxiety among first-generation immigrant Latino youth. Journal of Nervous and Mental Disease, 198(7), 470-477.
- Priest, N., Paradies, Y., Trenerry, B., Truong, M., Karlsen, S., & Kelly, Y. (2013). A systematic review of studies examining the relationship between reported racism and health and wellbeing for children and young people. Social Science & Medicine, 95, 115-127.
- Umaña-Taylor, A. J., Tynes, B. M., Toomey, R. B., et al. (2015). Latino adolescents’ perceived discrimination in online and offline settings: An examination of cultural risk and protective factors.Developmental Psychology, 51(1), 87-100.
EMERGING HEALTH NEEDS OF IMMIGRANT FAMILIES IN CALIFORNIA
In partnership with The California Program on Access to Care (CPAC), California Primary Care Association & and the 151 providers who participated in the survey, we’ve released a report on Emerging Health Needs of Immigrant Families in California.
HEALTHY MIND HEALTHY FUTURE WEBINAR
We held a webinar on August 7th to give you all an exclusive first look at our research findings before we release our report. Download the webinar to learn about our research findings, implications on the health and wellbeing of children in California, and opportunities for future advocacy. Feel free to share with your networks. #HealthyMindHealthyFuture
JOINT BLOG
Read our Executive Directors’ joint blog to learn more about our shared goals and our first-hand knowledge. As one is the daughter of Mexican immigrants and the other an immigrant from the Philippines, we take this work personally and take pride in the work we are doing to support children in immigrant families.
SHARE
To download: Right-click the desired image and choose Save Image.
Tweet: #California is home to 9 million #children, half of which have an immigrant parent. New @KidsPartnership report provides a health provider perspective on California’s children in immigrant families. https://bit.ly/2IMY61u
Tweet: Immigrant families have long endured trauma, anxiety & other longstanding negative health impacts due 2 unjust policies that separate families & go against American values of inclusion & equality. Learn about the health implications of these policies at: https://bit.ly/2IMY61u
Tweet: DYK: 90% of surveyed health care providers in #CA reported an increase in anxiety and fear, among children in immigrant families, due to detention and deportation. 50% of providers also saw an increase in anxiety and depression diagnosis. Learn more: https://bit.ly/2IMY61u
Tweet: @KidsPartnership commissioned a survey on #California’s #children in #immigrant families’ and their families access to care & overall #health. Findings highlight negative effects of federal anti-family and anti-immigrant policies. Learn more: https://bit.ly/2IMY61u