PARTNERSHIPS & COMMUNITY
We work with partners across the state to educate and enroll California families in quality, affordable health coverage. By partnering with leading education, health, immigrant, consumer, business, and advocacy organizations, we promote health coverage and enrollment for all children in California. We equip families with the information they need about coverage options and connect them to resources to help them enroll. Through high-impact partnerships, our ALL IN For Health Campaign brings new tools and information about health coverage and care opportunities directly into communities.
POLICY
We advocate policies that ensure all California children—regardless of their immigration status or family income—have access to the affordable, comprehensive health coverage they need to grow up healthy and ready to learn. We make sure that state outreach and enrollment processes, as well as other systems, work best for families. Using our work in California as a model, we advocate federal policies that help ensure children across the country have affordable, comprehensive health coverage.
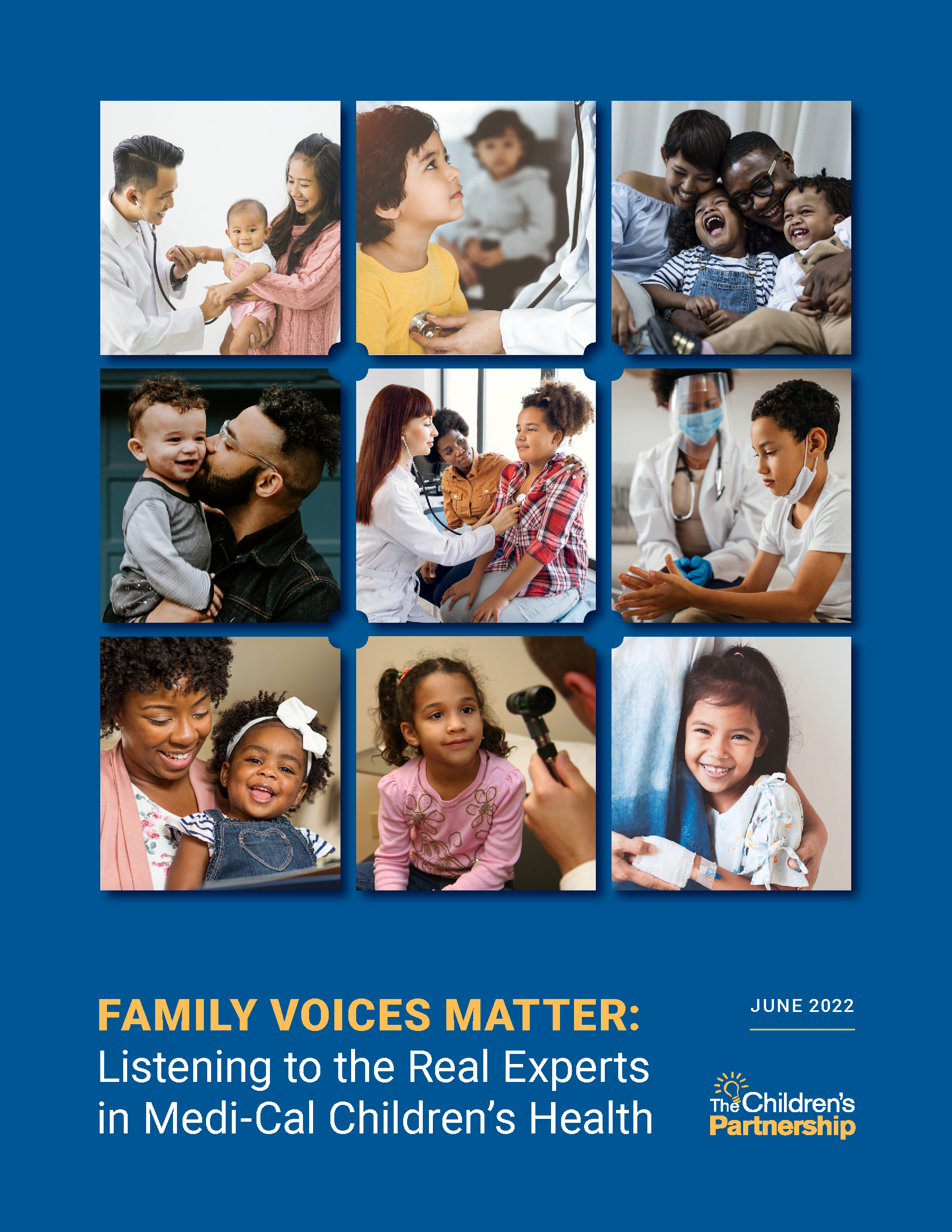
Caring for Kids The Right Way: Key Components of Children’s Care Coordination
In our new report, Caring for Kids the Right Way: Key Components of Children’s Care Coordination, a companion to our September 2021 Care Coordination for Children in Medi-Cal issue brief, we present successful children’s care coordination models and examples of care coordination in action. These models are essential to achieve the state’s ambitious goal of reforming the nation’s largest Medicaid program, and are necessary to address the well-documented challenges managed care plans have in offering preventive care and taking action on the social drivers of health.
When three out of four children in Medi-Cal are children of color, addressing social drivers of health offers a unique opportunity to advance equity but only when we center the needs of those most impacted.
Navigating the right support among the fragmented systems of children’s medical care is difficult, and successful care coordination for children requires effective communication among providers, patients and families across the multiple systems that serve children.
Family Voices Matter: Listening to the Real Experts in Medi-Cal Children’s Health
Because parents know their children and their lived experience best, their expertise is a critical component to integrate into any “whole-child” preventive care approach. Families’ input is important within their own child’s multidisciplinary care team, as well as in designing and implementing programs and policies affecting children’s health care. Bringing equity to children’s health starts with listening and sharing decisionmaking with the experts, namely the parents and families of children.
Because three-fourths of Medi-Cal children are children of color, Medi-Cal plays a critical role in addressing child health inequities and preventing children from developing diseases later as adults. However, Medi-Cal has not provided the well-child care and follow-up services federally required to be provided to children.
That’s why we turned to 58 parents representing the racial composition of Medi-Cal families to tell us where they go for help in navigating health care for their children and what Medi-Cal can do to improve health coverage and the delivery of care for their children. Our new report, Family Voices Matter: Listening to the Real Experts in Medi-Cal Children’s Health, is intended to provide parents’ perspectives about their experience with their children’s coverage and their suggestions for improving children’s health care and for how health plans can collaborate with families on systems change.
The Medi-Cal Managed Care Obligation for Care Coordination Couldn’t Be Clearer— It’s Time to Make It Work!
With Medi-Cal managed care plans (MCPs) providing coverage to 4.9 million California children, we have a historic opportunity to advance California children’s health care and health this year as DHCS will be reprocuring MCP contracts. Stakeholders have an opportunity to provide input into these draft contracts. Comments are due July 1.
In partnership with California Children’s Trust, we co-authored a Care Coordination Issue Brief as a snapshot of the current MCP care coordination obligation for all children enrolled in Medi-Cal. Care coordination is a critical linchpin between assessing and identifying socioemotional and health risks, as well as children getting health care and support services. This brief provides recommendations for care coordination improvement in Medi-Cal, including suggestions on strengthening MCP contract language and accountability to ensure California’s most vulnerable children are supported in navigating complex systems and multiple providers to receive the mental and behavioral health services they need.
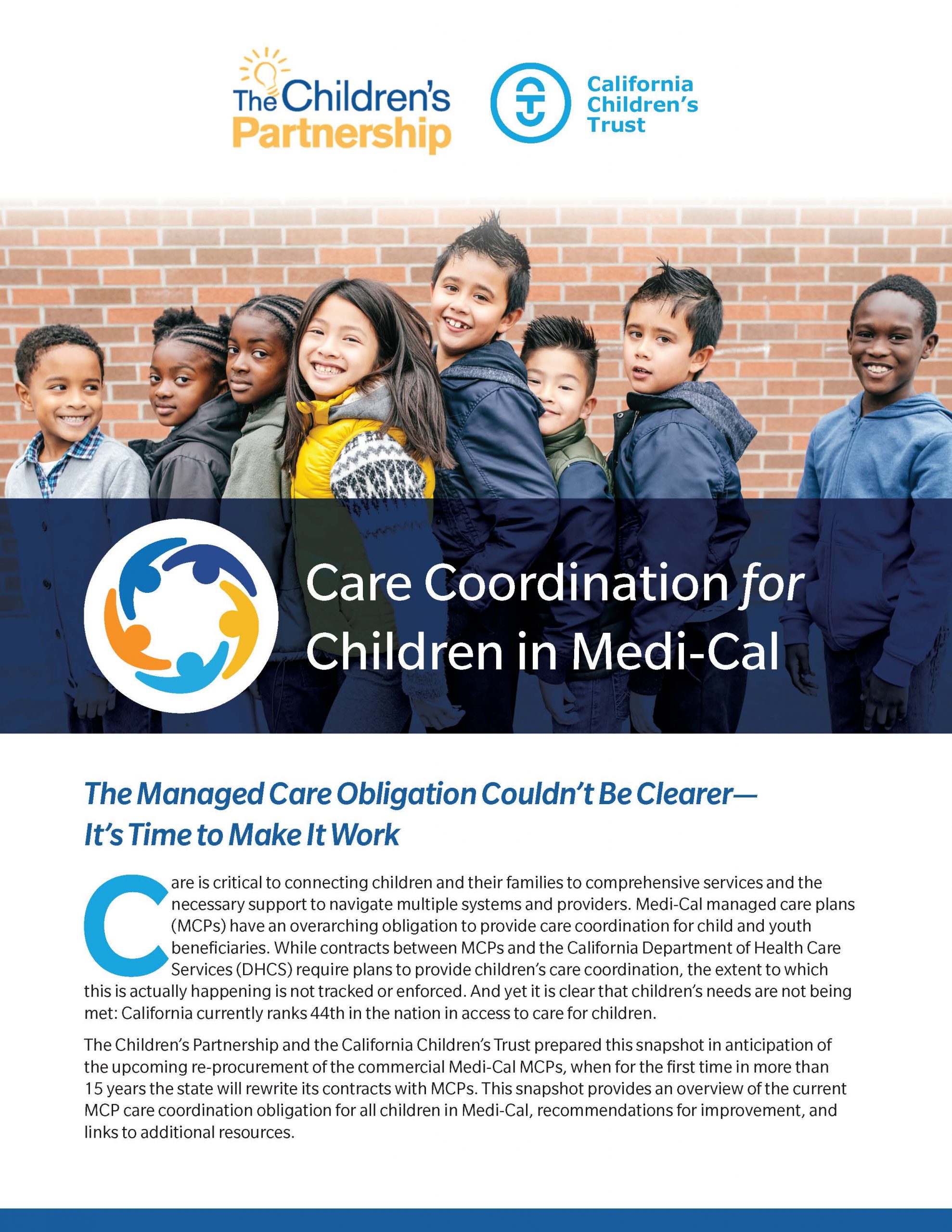
WHY IS CHILDREN’S ENROLLMENT IN MEDI-CAL LAGGING IN CALIFORNIA AT A TIME WHEN CHILDREN ARE IN MOST NEED?
Prior to the COVID-19 pandemic, the number of uninsured children increased for the first time in a decade. Since the pandemic began, when need of support has been at its highest, Medi-Cal enrollment for children has lagged. Children’s health care dropped off and has not fully bounced back, leaving gaps in vaccinations, well child visits and mental health care. Continuous coverage is essential to ensure children stay connected to health care. Read our newest fact sheet on Medi-Cal enrollment that highlights a few strategies California policymakers should consider to enroll more eligible children.