Racial Justice in Children’s Oral Health
In honor of National Children’s Oral Health Month, The Children’s Partnership (TCP) reaffirms our commitment to advancing race equity in all forms of health care, including oral health. Systemic racism is a root cause of children’s health inequities and must be centered in our health policy conversations. This blog explores the ways systemic racism shapes oral health inequities with recommendations and resources to help address it.
Good oral health is linked to long-term overall health and academic opportunity, however, caries–or tooth decay–remain the most common chronic disease among children in the United States, despite being preventable. In California, tooth decay is a significant public health problem, especially for young children. By the third grade, six in 10 children (61 percent) have experienced tooth decay and one in five children (22 percent) have untreated tooth decay.
However, the greatest burden of oral health issues continues to fall on children and youth from historically marginalized communities of color. Inequities by race, ethnicity and socioeconomic status for tooth decay and untreated decay are profound.
Inequities in Tooth Decay by Race and Ethnicity
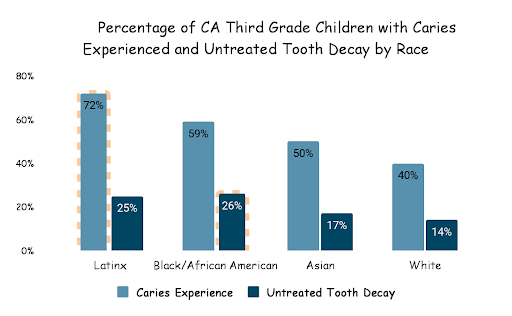
While California has made progress over the past years improving the oral health of children, data continues to show deep racial and ethnic divides when it comes to tooth decay. The findings from the 2018-19 California Smile Survey – released for the first time in nearly two decades – demonstrate a sharp divide based on race, ethnicity, language and socioeconomic status.
- Latinx children have the highest prevalence of tooth decay, with more than 72 percent who have experienced some form of tooth decay compared to 40 percent of white children.
- Black children have the highest prevalence of untreated tooth decay – over one in four (26 percent) of Black children had untreated tooth decay, nearly double the rate of white children (14 percent).
- Among Asian American children, 17 percent experience untreated decay and 50 percent experience tooth decay, compared to 14 percent and 40 percent of white children, respectively.
- Language disparities also impact the ability for children and families to access dental care. Tooth decay is more prevalent in children from Spanish speaking households (79 percent) compared to children in English speaking households (52 percent).
- Despite facing the greatest inequities, Latinx and Black children also have the lowest rates of accessing dental sealants – a protective coating that helps keep cavities from forming in the first place.
This data reflects systems that have not been structured to adequately serve the oral health needs of children of color. While tooth decay may be prevented through daily actions that minimize the development of decay, such as brushing two times a day with fluoridated toothpaste, drinking fluoridated water and avoiding sugar-sweetened beverages, changes in individual behaviors, alone, are not enough to address these systemic issues. Understanding these basic preventions is critical, but differences in access to providers and oral health services and resources, language and education make it more difficult for some parents and caregivers to access the tools needed to support their children’s oral health.
Root Causes Of Oral Health Inequities
Racism plays a key role in producing and sustaining oral health inequities by shaping the social conditions (social determinants of health) that are important to oral health, and by creating inequitable access to oral health services and the receipt of lower-quality oral health care. Poverty, food insecurity and inequitable access to critical resources like dental care and health coverage and receipt of lower-quality care all produce and sustain oral health disparities that disproportionately impact children of color.
For the five million children enrolled in Medi-Cal, the majority of whom are children of color (more than 75 percent), the negative effects of the socioeconomic determinants of health are exacerbated by the difficulty in locating dental professionals who accept Medi-Cal insurance coverage. A state audit report from 2014 found that nearly 56 percent of children enrolled in Medi-Cal did not receive dental care, at least in part because of an uneven distribution of dental providers, leaving some geographic areas with a significant lack of providers to meet the demand for care.
These challenges have particularly been compounded by the COVID-19 pandemic which resulted in the closure of several dental offices – further restricting children’s access to regular treatment and preventive services. In 2020, the numbers are even worse: only 34 percent of children and youth enrolled in Medi-Cal had at least one dental visit that year, and only 29 percent received preventive oral health services. While rates of dental care utilization have dropped among all children enrolled in Medi-Cal, data particularly shows Black children as the most affected, who received dental care at significantly lower numbers during the first year of the COVID-19 pandemic compared to all other children.
It is clear that California must do better in addressing root causes that continue to shape oral health inequities among children of color in our state, including by addressing systemic racism that exists within our systems and communities.
Use a Racial Justice Lens for Tooth Decay Prevention
In support of advancing a child health equity agenda, TCP has put forward policy briefs with recommendations that seek to reduce the disproportionate impact oral health inequities have on children of color through strategies that bring oral health care to where children spend most of their time (school), utilize technology to increase access to care, and integrate trusted community members who reflect the cultural and linguistic background of children and families facing the greatest inequities.
These strategies include virtual dental homes that use technology to bring safe, high-quality dental care to children where they already spend time: schools, early learning sites and other sites in the community; and early childhood caries oral health assessments conducted by trusted members of the community, like community health workers and promotores who help families navigate the health system and use technology to identify a child’s risk of experiencing dental disease and provide families with tailored education, resources and connections to care based on a child’s risk level.
Each of these examples centers the needs of children of color and their families through strategies that make it easier for them to identify health issues and access resources and care. Additionally, these examples highlight how community – both community based organizations and community members – is leading efforts to improve access to oral health care for children. Centering children, families and communities of color is critical to a racial justice lens as it allows those closest to the problem to lead the solutions.
Additionally, TCP is committed to ensuring that all families – regardless of their background – have the resources they need to understand and learn about the importance of oral health for their children – to place information and power in the hands of families. To help parents support their children’s oral health, in partnership with the Latino Coalition for a Healthy California, we developed a new fact sheet on why oral health matters, Bright Smile for a Bright Future: Children’s Oral Health in California. The fact sheet also highlights important information on Medi-Cal oral health services and dental coverage, as well as tips for parents to help their children have healthy teeth.
You can help us uplift the information in this fact sheet by using our social media toolkit here.
In order to build upon the progress California has made in lessening the burden of childhood tooth decay, we must continue to examine and address oral health inequities through a racial justice lens. It is clear that investments in oral health care must prioritize children and families of color. If we are to transform our health care system into one that truly responds to children and their unique needs, we must include oral health strategies that focus on prevention as well as a system of care that centers community leadership in oral health care delivery.